Nephrology
Case A :
A 52 yr old male patient who is a farmer by occupation ,Presented to hospital on 19 May 2021 with Chief Complaints of
SOB since 4 days
Burning micturition since 4 days
Questions :
1 . What could be the reason for his sob ?
A) The high creatinine levels and low sodium levels in blood indicates ... the kidney failure
B) The acute kidney failure altering the homeostasis of fluid balance , acid base balance and vascular tone...
C) this may lead to increasing pulmonary vascular permeability
D) which causes pulmonary edema ... which is fluid in lungs .
This causes shortness of breath
2. Why does he have intermittent episodes of drowsiness?
As the patient consider to have hyponatremia....
The symptoms of hyponatremia are lethargy fatigue and drowsiness
And the patient also know case of diabetes type 2 ... which may also cause drowsiness
Because of the imbalance between ones level of blood glucose and effectiveness of circulatory insulin
3. Why did he complaint of fleshy mass like passage in his urine ?
Fleshy mass like passage in urine can be seen because of the injury caused by medical tools...
He was post TURP patient... soo there may be chance of injury of medical tools...
4. what are the complications of TURP that he may have had ?
i) He had infections ... because of which there is an high grade fever and burning micturition
ii ) he had electrolyte imbalance ..... because of which he had hyponatremia
Case B:
AN 8-YEAR-OLD BOY WITH FREQUENT URINATION
The informant is the mother, who complained that her son urinates frequently i.e, about 25 times /day.
1) why is the child excessively hyperactive without much social etiquette?
Ans: From the history of excessive hyperactivity, impulsiveness, lacking attentivity,a thought goes towards attention deficit hyperactivity and in association urination disorders.
2)Why doesn't the child have excessive urination at night time?
Ans: since the child does not get the urge to urinate when he is asleep, there can be a chance of manifestation being psychosomatic, or as a result of an undiagnosed anxiety disorder.
3)How would you want to manage the patient to relieve him of his symptoms?
Ans: daytime overactive bladder is a common pediatric problem that usually resolves over time which usually resolves over time with reassurance and relaxation and behavioral therapy.
Cardiology :-
Case A :
A 78 yr old male patient, resident of of kattangur and shepherd by occupation came to the Opd on 14 /5/2021 with chief complaints of :
SHORTNESS OF BREATH ,SINCE 20 DAYS
CHEST PAIN ,SINCE 20 DAYS
B/L PEDAL EDEMA , SINCE 4 DAYS
FACIAL PUFFINESS , SINCE 4 DAYS
1. What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
A) Heart failure is when heart cannot maintain adequate output, or can do so only at the expense of elevated ventricular filling pressure
B) cardiac output = heart rate × stroke volume
C) ejection fraction is percentage of end diastolic volume which ejected per contraction or stroke from each ventricle
Which is one of the factor that determine the stroke volume ...
D ) heart failure with preserved ejection fraction occurs when left ventricle is not filled completely in diastolic phase
The blood pumped out is less
Causes diastolic heart failure
E ) heart failure with reduced ejection fraction occurs when muscle of left ventricle is not pumping well as normal
The amount of blood pumped out is less than body needs ... causes heart failure
2.Why haven't we done pericardiocenetis in this pateint?
His haemoglobin values and pallor on examination indicates... she has anemia
Where there will be excess blood loss in pericardiocenetis process ... so we didn't done that
3.What are the risk factors for development of heart failure in the patient?
A) infections
B) NSAIDS
C) Anaemia
D) arrhythmia
E) Thyrotoxicosis
F) infective endocarditis
G) myocarditis
H) myocardial infraction
I) pulmonary embolism
4. What could be the cause for hypotension in this patient?
Soo may be the pericardial effusion causes the hypotension
Case B :
A 73 yr male patient teacher by occupation, resident of .............. presented to Opd with chief complaints of :
- PEDAL EDEMA ,SINCE 15 DAYS
- SHORTNESS OF BREATH, SINCE 4 DAYS
- DECREASED URINE OUTPUT ,SINCE 2 DAYS
1. What are the possible causes for heart failure in this patient?
I ) the fever, and ulcer indicates... there is an infection in the body... which may lead to ulcer
ii ) the infection may lead to decrease in cardiac output
III ) he has anemia .. which can also lead to heart failure
2.what is the reason for anaemia in this case?
The patient has chronic kidney disease (ckd)
Where kidney function is reduced..... because of that the kidney can't produce the Erytropoitine.... which causes anemia
3. What is the reason for blebs and non healing ulcer in the legs of this patient?
The diabetes is one of the causes for leg unclers. Because of high blood sugar .... there is delay in healing...
The leg uncer may also occur due anemia
Pulmonology
Case 1:
A 55 year old female patient, a resident of Miryalaguda and farmer by occupation came to the hospital on 17/5/21 with the chief complaints of shortness of breath, pedal edemaand facial puffiness.
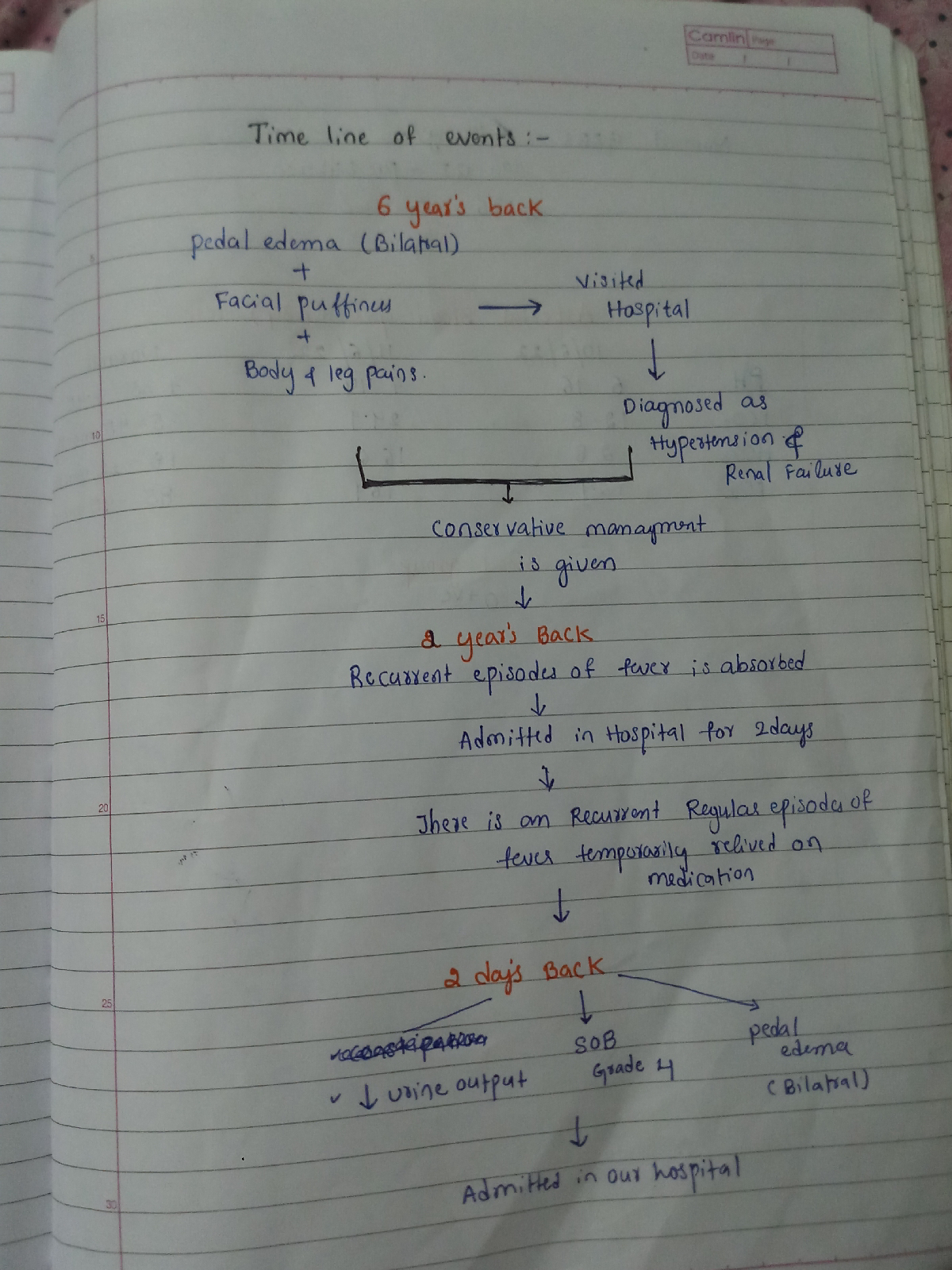
1Q) what is the evolution of the symptomatology in this patient interms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient problem ?
Evolution of symptomatology
1st episode of sob - 20 yr back
2nd episode of sob - 12 yr back
From then she has been having yearly for the past 12 yrs
Diagnosed with diabetis - 8yrs back
Anemia and took iron injections - 5yr ago
Generalised weakness - 1 month back
Diagnosed with hypertension - 20 days back
Pedal edema - 15 days back
Facial puffiness- 15 yrs back
Anatomical location of problem - lungs
Primary etiology of patient- usage of chulha since 20 yrs might be due to chronic usage
2)what r the mechanism of action indication and efficacy over placebo of each of the phramacological and nonphramacological interventions used for this patient?
Head end elevation :# MOA;
.improves oxygenation
.decreases incidence VAP
.increases hemodynamic performance
.increases end expiratory lung volume
.decreases incidence of aspiration
#Indication: .head injury
.meningitis
.pneumonia
oxygen inhalation to maintain spo2
Bipap:non invasive method
#MOA :assist ventilation by delivering positive expiratory and inspiratory pressure with out need for ET incubation9
3. Cause for current acute excerbation
it could be due any infection
4.could the ATT affected her symptoms if so how?
Yes ATT affected her symptoms
Isoniazid and rifampcin -nephrotoxic - raised RFT was seen
Infectious diseases and hepatology
Case 7 (A)
A 55 year old male patient who is a palm tree climber by Occupation came on 17th April 2021 with the chief Complaints of
PAIN ABDOMEN SINCE ONE WEEK DECREASE APPETITE SINCE ONE WEEK FEVER SINCE 2 DAYS
1Q)do u think drinking locally made alcohol cause liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient?
yes, it could be due to intake of contaminated toddy
2Q)what is the etiopathogenesis of liver abscess in a chronic alcoholic patient?(since 30 yrs - 1 bottle/day)
- according to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess.
3Q)is liver abscess is more common in right lobe?
yes right lobe is involved due to its moreblood supply
4Q) what r the indications for usg guided aspiration of liver abscess
Indications for USG guided aspiration of liver abscess
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
Case 8 ( A) :
50/Male who is a resident of choutuppal
Daily wage labourer by occupation
Came with cheif complaints of
Fever since 10 days
Facial puffiness and periorbital edema since 4 days
Weakness of right upper limb and lower limb since 4 days
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans:
18/04/21 He went to local PHC for COVID 19 vaccination.. Since that night patient is complaining of Fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication...
No c/o cold and cough
Followed by patient is having similar complaints after three days and he visited local hospital which is not subsided by medication ( Antipyretics) ( not taken medication such as steroids, oxygen therapy, anti virals)
On 28/04/21 , c/o Generalized weakness and facial puffiness and periorbital edema.. And also patient is in drowsy state..
On 04/05/21, patient presented to casualty In altered state with facial puffiness and periorbital edema and weakness of right upper limb and lower limb...
primary etiology: Diabetes can lead to mucormycosis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Proposed management -
Inj. Liposomal amphotericin B according to creatinine clearence
Loading dose 30mg/IV over 2-6 hrs
Maintenance dose 60mg / IV once a day
Treatment modalities:
The successful treatment of mucormycosis requires four steps: 1) early diagnosis; 2) reversal of underlying predisposing risk factors, if possible; 3) surgical debridement where applicable; and 4) prompt antifungal therapy [3].
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Thus far, this surge has been attributed to the improper use of steroids to treat Covid-19 patients, coupled with poorly managed diabetes. But steroids in themselves are not the villains.
“Systemic (oral and intravenous) corticosteroids have been proven to reduce mortality in Covid-19,” Lancelot Pinto, consultant pulmonologist at Mumbai’s Hinduja Hospital, told Quartz. “The largest trial, Recovery, which proved this beyond a reasonable doubt among individuals who had low oxygen levels, used them in a dose of 6 milligrams Dexa per day for up to 10 days.”
Not only in Covid-19, but steroids are also widely used in orthopaedic and pulmonary diseases. In India, the problem lies not in the drug but in how it is prescribed. “Most of us who work in India will agree that prescribing practices more often than not tend towards higher doses for longer periods of time, which is a clear risk factor for invasive fungal infections
Medicines used in treating Covid-19 tend to bring down the count of lymphocytes. Lymphocytes are one of the three types of white blood cells whose job is to defend our body against disease-causing pathogens such as bacteria, viruses, and parasites. The reduced count of lymphocytes leads to a medical condition called lymphopenia, making way for opportunistic fungal infection in Covid-19 patients.
There is a higher chance of occurrence of mucormycosis in patients whose immune system is not functioning well, and since Covid-19 treatment tends to suppress the working of the immune system, it places such patients at a higher risk of contracting the black fungus infection
Case 6 (A) :
A 40 year old lady who works in cotton fields came to the hospital with the chief complaints of :
- DIFFICULT IN SWALLOWING,FEVER AND COUGH, SINCE 2 MONTHS
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Answer: Tracheoesophageal fistula is suggested by copious salivation associated with choking, coughing, vomiting, and cyanosiscoincident. Esophageal atresia and the subsequent inability to swallow typically cause polyhydramnios in utero.
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Answer: There are chances that patient may develop IRIS. The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
Gastroenterology and pulmonary
Case 4 ( B ) :
A 25 year old man,daily wage worker and tractor driver by occupation, presented with:
•Severe abdominal pain since 4 days
•One episode of vomiting 2 hours before presenting to hospital
•Shortness of breath on walking since 2 hours
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
A) Inflammatory cells caused dyspnea
B) With pancreatitis there are a lot of inflammatory chemicals that are secreted into the blood stream. These chemicals create inflammation throughout the body, including the lungs.
2 )Name possible reasons why the patient has developed a state of hyperglycemia.
According to the patient history the he is a chronic alcoholic
- alcohol consumption can interfere with blood sugar as well as the hormones needed to maintain healthy blood sugar levels
- Chronic alcohol consumption can reduce the overall effectiveness of insulin which results high blood sugar levels ( hyperglycemia)
- Other reasons for hyperglycemia May arise from mechanism such as uncontrolled pre-existing Diabetes mellitus ,damage to endocrine pancreas to severe attack of acute pancreatitis
3)What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
- Elevated liver function test especially ALT and Bilirubin level may be suggestive of CHOLIDOCHOLITHIASIS (Gallstones in common bile duct)
- Biochemical markers for chronic alcohol consumption that have been most commonly studied are serum GGT AST ALT MC
4)line of treatment in this patient?
- Supportive therapy like IV Fluids to prevent dehydration
- GRBSmonitoring
- Analgesics to relieve pain
- Procedures to remove bile duct ER CP which helps in diagnosing problems in bile and pancreatic duct
- Antiemetics and treatment of underlying cause and treatment for alcohol dependence
Neurology
Case G :
A 50 year old patient with cervical myelopathy
A 50 year old male patient presented to hospital with complaints of weakness of all four limbs since 8pm.
No h/o slurring of speech.
No h/o fever.
1)what is myelopathy hand?
Ans: The loss of power of adduction and extension of ulnar two or three fingers and an inability to grip and release with these fingers.
2)what is finger escape?
Ans:hold fingers adducted and extended.
Small and ring fingers fall into flexion abduction,usually within 30 seconds.
3) what is Hoffman's reflexe?
Ans: Hoffman's reflex is a neurological examination finding elicited by a reflex test which can help verify the presence or absence of issues arising from corticospinal tract.
Procedure:it involves loosely holding the middle finger and flicking the finger nail downward, allowing the middle finger to flick upward reflexively.A positive response is seen when there is flexion and adduction of the thumb on the same hand.
Case F:
30 yr old male patient with weakness of right upper limb and lower limb
1) weakness of right upper limb and lower limb
2)deviation of the mouth towards left since one day
1) does the patient's history of road traffic accident have any role in his present situation?
Ans: The patient has an ischemic cerebrovascular accident which is caused due to his stressful conditions and the lipid profile which has high LDL levels and low HDL levels--leading to narrowing of middle cerebral artery. the history of the accident has no role in his present situation.
2)what are the warning signs of a cerebrovascular accident?
1) sudden numbness or weakness of face, arm leg, especially on one side of the body
2)sudden confusion, trouble speaking or understanding
3)sudden trouble seeing
4)sudden trouble walking,dizziness, loss of balance
5)sudden, severe headache with no known cause.
3)what is the drug rationale in cva?
Ans :Mannitol: osmotic diuretic, decreases the intracranial pressure
phenytoin: antiepileptic
monocef: antibiotic
amlodipine: AntiHTN
citicoline:neuroprotective
aspirin: antiplatelet
Atorvastatin:antihyperlipidemic
4)Does alcohol has any role in his attack?
Ans: As the patient is daily drinker alcohol has a synergistic effect on worsening the ischemia due to liver damage, which decreases the production of substances that reduce the effect.
5)does his lipid profile have any role in his attack?
Ans :the patient have high LDLlevels and low HDL levels which have lead to narrowing ofmiddle crebral artery.
Case H :
A 17 year old female student by occupation presented to causality on 1/5/2021 with
Chief complaints of
1.Involuntary movements of both upper and lower limbs a day before.
1) What can be the cause of her condition ?
According to MRI cortical vein thrombosis might be the cause of her seizures.
2) What are the risk factors for cortical vein thrombosis?
Infections:
Meningitis, otitis,mastoiditis
Prothrombotic states:
Pregnancy, puerperium,antithrombin deficiency proteinc and protein s deficiency,Hormone replacement therapy.
Mechanical:
Head trauma,lumbar puncture
Inflammatory:
SLE,sarcoidosis,Inflammatory bowel disease.
Malignancy.
Dehydration
Nephrotic syndrome
Drugs:
Oral contraceptives,steroids,Inhibitors of angiogenesis
Chemotherapy:Cyclosporine and l asparginase
Hematological:
Myeloproliferative Malignancies
Primary and secondary polycythemia
Intracranial :
Dural fistula,
venous anomalies
Vasculitis:
Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.