medicine long case
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
55 years old female patient resident of choutuppal who have sedentary life came to the hospital on 10/6/22 with
Chief complaints:
-Shortness of breath Since 2 days
-Bilateral pedal edema since 2 days
-Decreased urine output since 2 days
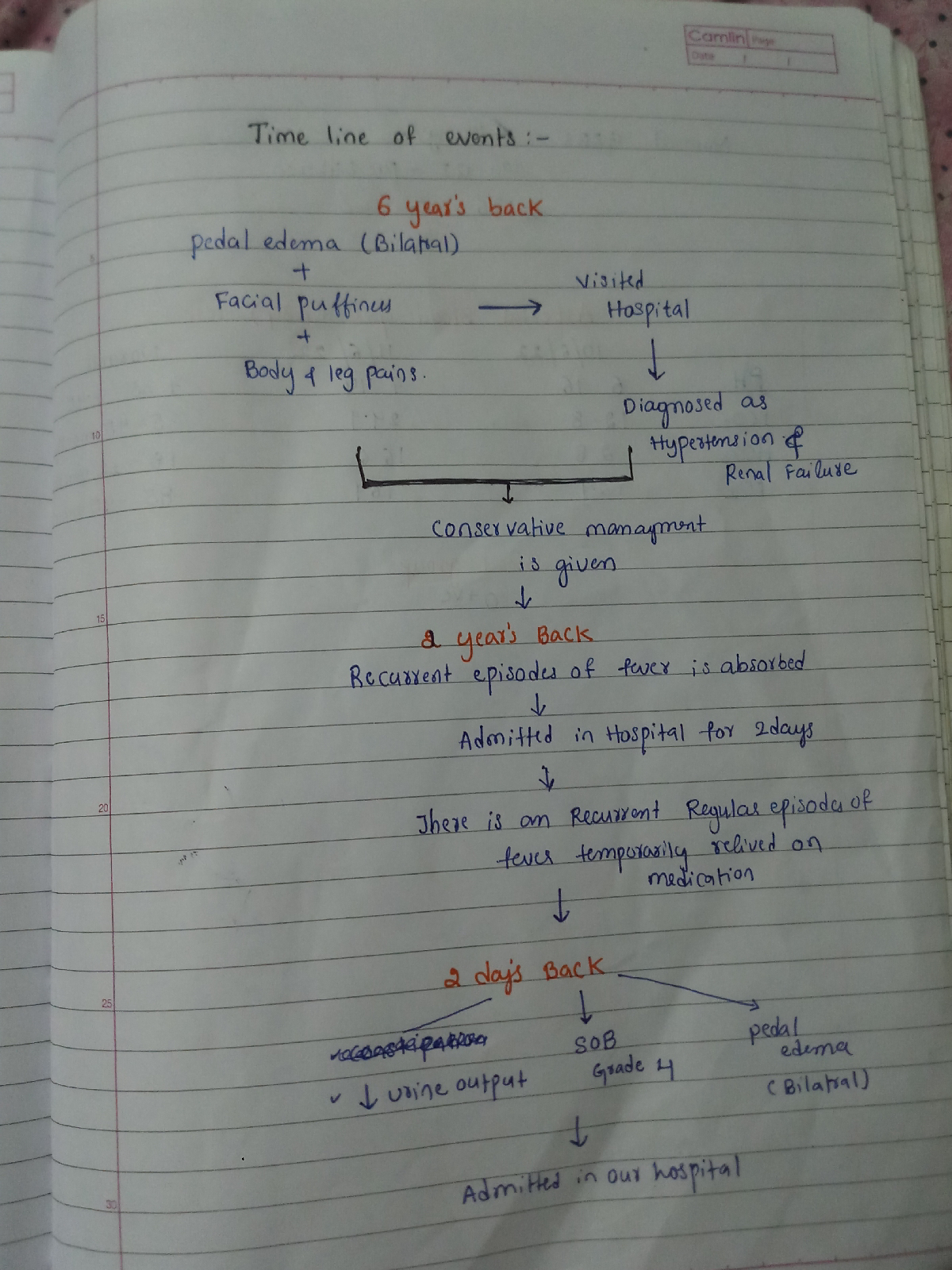
Time line of events:
HISTORY OF PRESENTING ILLNESS:-
Personal history:
Diet -mixed
Appetite -normal
Sleep -adequate
Bowelmovements-irregular since 2 days
Bladder movements-decreased urinary output since 2days
No known drug or food allergies
No addictions
Family history:
No significant family history
General examination:
After taking consent ,patient is examined in well lit room
Patient is conscious, coherent and cooperative well oriented to time ,place and person
moderately built and moderately nourished
Pallor- present
Icterus -absent
Clubbing -absent
Cyanosis -absent
Generalised lymphadenopathy -absent
Edema- present
Temperature-afebrile
Pulse rate -106 beats per minute ,regular rhythm ,normal volume,normal character ,no radio radial delay
Blood pressure -160/80mmHg measured in left arm in supine position
Respiratory rate -34 cycles per minute
SpO2- 92 %at room air
Respiratory system:
Upper respiratory system - normal
Examination of chest-
Inspection:
Shape of the chest -normal, bilaterally symmetrical
Trachea -central in position
Respiratory movements -normal, bilaterally symmetrical
No scars,sinuses, engorged veins seen on chest wall
Palpation:
No local rise of temperature
No tenderness
All inspectory findings are confirmed
Trachea -central in position
vocal Fremitus - normal
Chest movements - normal ,symmetrical bilaterally
Percussion:
Resonant note heard
Auscultation:
Bilateral air entry present
Normal vesicular breath sounds heard
Bilateral basal crepitations heard at infrascapular and infra axillary
Cardiovascular system :
S1 S2 heard , no added sounds are heard , no murmurs are heard
Abdominal examination:
Per abdominal- normal and non tender , no Organomegaly
Central nervous system examination-